Pumping Breast Milk 101
|
8 min
|
8 min
Many mothers pump breast milk for their babies at some point during their breastfeeding journey. There are a variety of reasons for pumping milk, including helping with the establishment of the milk supply when there are challenges in the beginning, increasing the milk supply, having milk to leave for your baby while away, or working, exclusively pumping your milk to provide for your baby, or to build a small “just in case” stash. Pumping looks different for everyone, depending on the reason for pumping and their baby’s needs.
During pregnancy, the breasts undergo changes to produce and store milk for the newborn baby. Colostrum begins to be produced as early as 12-16 weeks during pregnancy and may begin to leak in the 3rd trimester. (1) As estrogen increases, milk ducts are developed, and the secretion of prolactin is signaled. Higher progesterone levels are responsible for milk-making cells to form and grow.
Breast changes in pregnancy:
After your baby is born, the placenta is delivered, causing progesterone and estrogen to drop. This drop signals Prolactin, the hormone responsible for making milk, to increase and for milk production to increase. Over the next 2-3 days, your milk will transition from colostrum to mature milk. Colostrum is very concentrated compared to mature milk, which is abundant in volume.
Keep your baby skin-to-skin, beginning within the first hour after birth, and offer the breast often. Hormones drive this stage of lactation. Milk will be made even if milk is not being removed. How often your baby nurses and how much milk is removed each feeding is essential during this stage. When milk is removed, prolactin signals for more milk to be made. If the breast remains full of milk, it signals to slow down milk production. Feeding your newborn often means more times milk is removed and more refilling of milk occurs. If your baby goes to the breast frequently but is not removing sufficient milk, production is also affected. Without adequate and frequent milk removal, some of the cells that hold milk will begin to shut down. (2) Around 10 days postpartum, milk supply begins to be driven by demand.
Not all parents need to pump. You don't need to include pumping if you will be with your baby for every feeding.
Beginning to pump too soon can signal higher milk production and lead to an oversupply. You are meant to produce the amount of milk needed for your baby. Having too much milk can make you and your baby uncomfortable.
How often you will be away from your baby will determine your pumping and milk-storing needs.
Occasional separations:
Milk production remains fairly constant from about 6 weeks until the introduction of solid foods. Your baby eats about 24- 30 oz per 24 hours, taking 2 - 4 oz per feeding. (4) Most parents like to store enough milk for 2 days away from the baby to have a little cushion of extra milk.
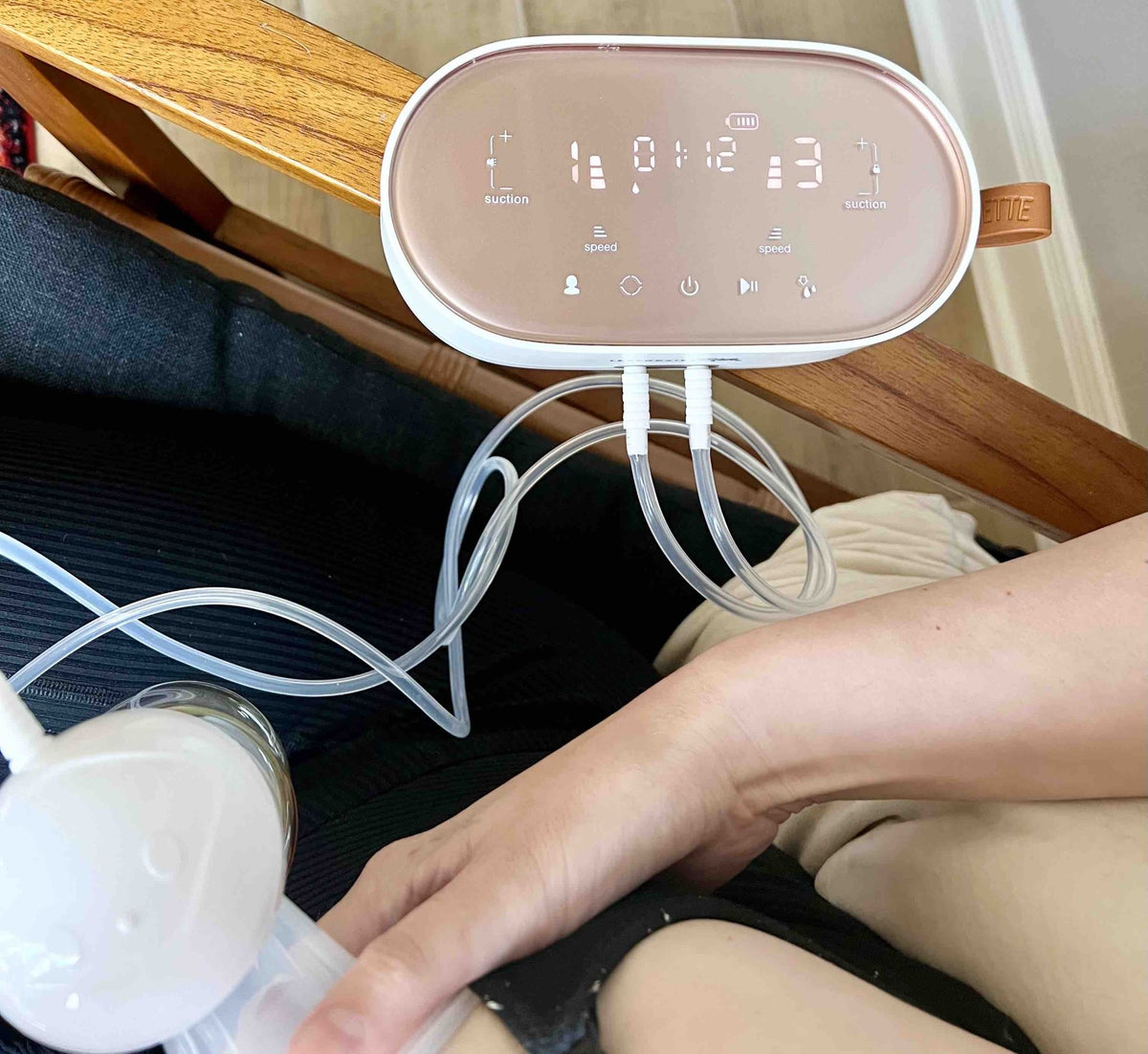
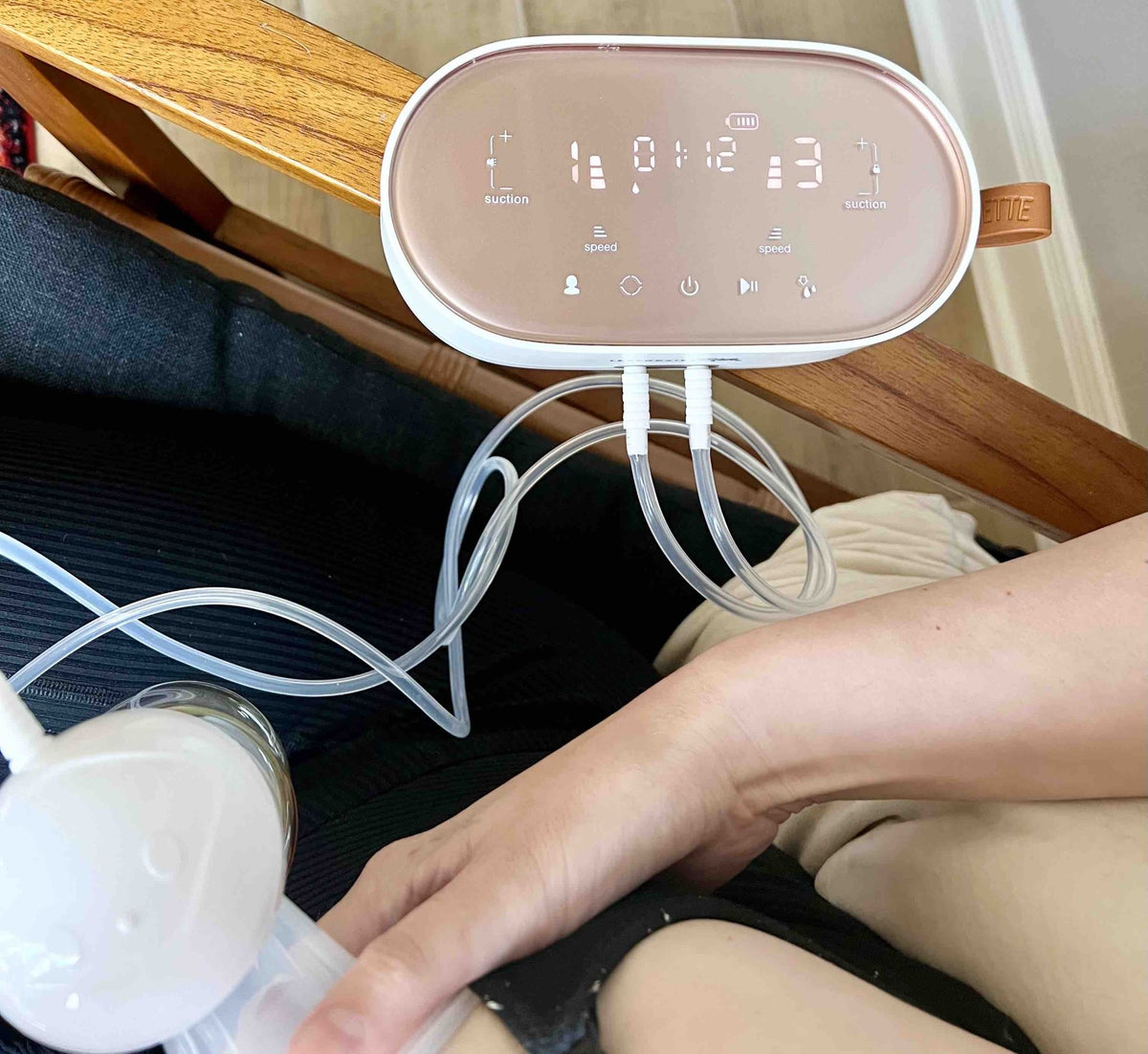
A double electric pump is often the most effective way to collect milk if you need to pump for returning to work. Many options are available, including hands-free collection cups to make pumping more convenient when your hands need to be free or taking a break at work is challenging.
The Legendairy Milk Duette is a dual electric breast pump with a variety of individual speeds and suction levels for each breast to customize your pumping experience.
To determine how much milk you need to pump and leave for your baby while you are away from them, estimate how many times your baby nurses in 24 hours and divide that by the average amount of milk they drink daily, which varies between 24 - 30 ounces. You can use 25 ounces as an average. This will give you the amount per bottle. Plan on one bottle every 2-3 hours while away.
Example: 25 ounces divided by 10 feeds per 24 hours = 2.5 ounces
Example: 30 ounces divided by 10 feeds per 24 hours = 3 ounces
The amount of milk you are able to pump is dependent on how old your baby is, what time of day you pump, when you last nursed or pumped, and your breast storage capacity.
The average amount to expect from pumping during a regular pumping session is 3 - 4 ounces. (6) If you are pumping between feeds, the amount may be closer to 1.5 - 2 ounces.
Pump Parts
Ensure all your pump parts are working properly. Some parts will need to be replaced more frequently than others. How often you replace them depends on how often you are pumping. The guidelines below are based on pumping 3 or more times a day and less than 3 times per day. The more often you pump, the sooner the parts will wear out.
Flange Fit
Pumping should be comfortable and never hurt. If a flange is too big or small, it can be uncomfortable and cause damage to the nipple and areola. If the shield/flange is the wrong size, it will not be as effective at removing milk and can affect your milk supply over time. If you’re taking the time to pump, you want to get the most milk possible.
Flange/shield size can change over the course of nursing. A nipple ruler can be a helpful tool for finding your correct flange size. Many IBCLCs (International Board Certified Lactation Consultants) offer Flange Fitting Consults.
Using a lubricant on your breast shield/flange, like Legendairy Milk Pumping Spray , can add comfort while pumping, and the oils nourish your skin.
Expressing Your Milk
It can take time and practice pumping for your body to respond to the pump. It is common not to see immediate results.
Here are some techniques that can help:
Milk quality does degrade the longer it is in the freezer, so it is best only to store what you will need for your baby for a couple of days in most circumstances. (7) Store newly pumped milk in the back of older pumped milk so you grab the older pumped milk to give your baby first.
Learning about pumping can seem overwhelming at first. Having some basic tips and facts about what to expect can help make it easier. Experimenting is part of the process of finding what works best for you and your baby. Using flanges that fit you best, replacing pump parts as needed, and using hands-on techniques while pumping help you get more milk out at your pump sessions. Remember, your IBCLC is always available if you need a little extra guidance or a plan for making pumping work for you.