The Breast Microbiome & Maternal-Infant Health: Dysbiosis, Mastitis, and the Tools to Support Balance
|
6 min
|
6 min
Breastfeeding is an incredible journey not only for your baby but for your own body as well. One of the most exciting emerging areas of research in lactation is the breast microbiome: the community of beneficial bacteria found in breast tissue, ducts, and human milk. Far from being sterile, breast milk contains living microbes that protect the breast, support healthy lactation, and help establish your baby’s gut microbiome (1).
When the breast microbiome is balanced, it supports both maternal and infant health. But when it becomes disrupted, or what researchers call dysbiosis, issues such as clogged ducts, inflammation, and bacterial mastitis can occur. Understanding the breast microbiome, how it influences your baby’s gut, and the role of supportive tools like Lacta-Biotic® and Sunflower Lecithin can empower you to nurture your microbial health while protecting your breastfeeding journey.
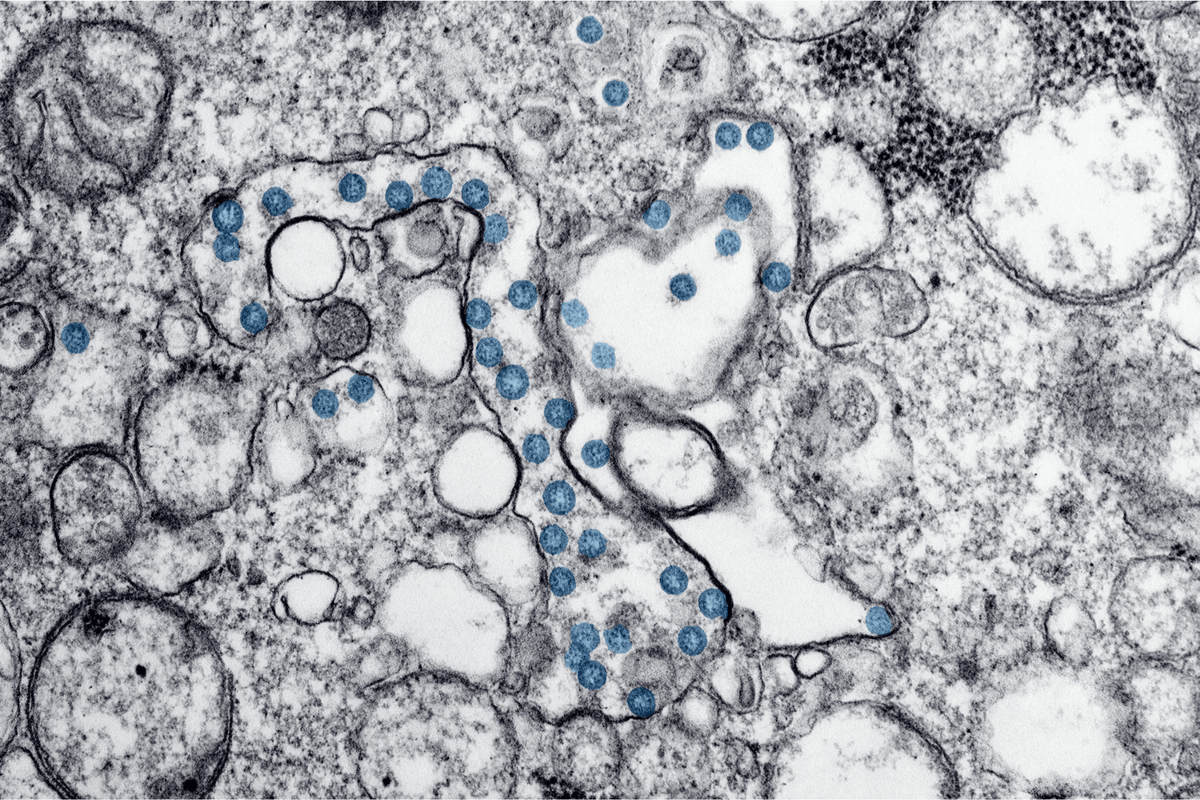
The breast microbiome is made up of a diverse community of bacteria, including Staphylococcus, Streptococcus, Lactobacillus, and Bifidobacterium (1). These microbes come from multiple sources, including the maternal gut, the infant’s mouth, and the surrounding skin. The pathway from the maternal gut to the mammary gland is often called the entero-mammary pathway, and it allows maternal gut bacteria to translocate into breast milk, where they may benefit the infant (2).
A healthy breast microbiome is diverse and balanced. This microbial balance helps prevent infections, promotes healthy milk flow, and provides beneficial bacteria that directly support the infant gut microbiome.
Dysbiosis refers to an imbalance in the microbial community. In the breast, dysbiosis often means that beneficial bacteria decrease, while potentially pathogenic bacteria such as Staphylococcus aureus overgrow. This imbalance increases the risk of conditions like clogged ducts and mastitis.
Mastitis can develop when milk flow is obstructed and bacteria multiply, leading to painful inflammation. Symptoms may include localized pain, redness, swelling, and sometimes fever or flu-like symptoms. A recent review highlighted how breast dysbiosis is closely linked to the onset and persistence of lactational infective mastitis (3).
Risk factors for dysbiosis and mastitis include:
Cesarean delivery compared to vaginal birth (4)
Maternal antibiotic use during or after birth (4)
Maternal stress, diet, and lifestyle (1)
Infrequent or incomplete milk removal (5)
Addressing these risk factors where possible, alongside supportive preventatives and interventions, can help reduce recurrence.
One of the most important roles of the breast microbiome is how it contributes to the infant gut microbiome. Research shows that bacteria present in breast milk help seed the infant’s digestive tract, where they shape immune development and protect against pathogens (2,6).
Infants who receive breast milk with a diverse microbial community tend to have more balanced gut microbiota compared to those who do not (6). Human milk also contains human milk oligosaccharides (HMOs), complex sugars that act as prebiotics, feeding beneficial gut bacteria such as Bifidobacterium (7). Together, breast milk bacteria and HMOs create a microbial foundation that influences the baby’s digestion, immune system, and possibly even long-term health.
When milk flow slows, fat globules can clump, and ducts may become obstructed. This mechanical blockage provides an environment where bacteria can overgrow, increasing the risk of mastitis (5).
Clogged ducts can be painful and frustrating, often presenting as hard, tender lumps. If left untreated, they may progress to infection. Standard prevention strategies include frequent and effective milk removal, varied nursing positions, and ensuring a deep latch (5).
Because the breast microbiome plays such an important role in both maternal and infant health, supporting its balance is key. While clinical treatment may be necessary for mastitis, research is increasingly pointing toward supportive tools that may help maintain microbial balance and reduce recurrent issues.
Probiotics are live microorganisms that can restore balance to microbial ecosystems. Certain strains, such as Lactobacillus fermentum and Lactobacillus salivarius, have been studied for their potential to reduce mastitis incidence and symptoms (8). These probiotics are thought to work by competing with harmful bacteria, reducing inflammation, and supporting immune regulation within the breast.
Lacta-Biotic® was designed with these findings in mind, featuring probiotic strains that may help protect the breast from dysbiosis and support overall breast health during lactation. Clinical evidence is still emerging, but the available data suggest probiotics may be a safe and effective option to reduce mastitis recurrence (8).*
Sunflower Lecithin is another supportive tool frequently recommended by lactation consultants. Lecithin is a natural emulsifier, and supplementation may reduce the “stickiness” of milk fat, making it less likely to clump together and form blockages (9).*
For mothers experiencing recurrent clogged ducts, daily Sunflower Lecithin (typically 3,600–4,800 mg/day) has been suggested as a preventative strategy (9,10). Lecithin is considered safe for breastfeeding mothers, as it is a normal component of human milk and has minimal reported adverse effects (10).
By improving milk flow, Sunflower Lecithin can reduce the mechanical stress that contributes to clogged ducts and mastitis.*
While the breast microbiome is critical, it does not exist in isolation. Much of its bacterial diversity is linked to the maternal gut microbiome. Researchers have described an “entero-mammary pathway,” where maternal gut bacteria translocate to the mammary gland through immune cells, eventually appearing in breast milk (2). This means that the composition of your gut microbiome can directly influence the microbial landscape of your breast and the bacteria your baby receives.
Source of beneficial bacteria: The gut is a reservoir of Lactobacillus, Bifidobacterium, and other commensal strains that may seed breast milk and, in turn, colonize the infant gut (2).
Immune regulation: A healthy gut reduces systemic inflammation, which may help protect the breast from infection or severe mastitis (11).
Metabolic and hormonal interactions: The gut microbiome influences digestion, nutrient absorption, and metabolite production, all of which can affect maternal energy, milk supply, and resilience during lactation (12).
Eat a diverse, fiber-rich diet with fruits, vegetables, legumes, and whole grains.
Incorporate fermented foods such as yogurt, kefir, or sauerkraut. Consider probiotic supplements.
Prioritize rest and stress reduction, as the gut-brain axis links stress directly to microbial balance.
Use antibiotics thoughtfully, and replenish gut flora after necessary courses.
By caring for your gut, you are also nurturing your breast microbiome and setting the foundation for your baby’s microbiome.
The breast microbiome is an often-overlooked but vital part of breastfeeding. When it is balanced, it supports your breast health and helps establish your baby’s gut microbiome. When disrupted, it may lead to challenges such as clogged ducts or mastitis.
Tools like Lacta-Biotic® and Sunflower Lecithin offer supportive options to maintain microbial balance and reduce recurrence of problems. Alongside frequent milk removal, a nourishing diet, rest, and professional support, they can help keep your breastfeeding journey healthier and more comfortable.
Ultimately, the maternal gut, breast, and infant gut form a connected ecosystem. By supporting each piece of the puzzle, you nurture your own health while building the foundation for your baby’s lifelong wellness.
Notarbartolo, V., et al. (2022). Composition of human breast milk microbiota and its role in infant health. Frontiers in Microbiology, 13:9110848. https://pmc.ncbi.nlm.nih.gov/articles/PMC9110848/
Davis, E. C., et al. (2022). The gut microbiome and breast-feeding: Implications for early-life health. Frontiers in Immunology, 13:9463492. https://pmc.ncbi.nlm.nih.gov/articles/PMC9463492/
Pathak, P., et al. (2024). The association between lactational infective mastitis and the microbiome: Development, onset, and treatments. Cureus, 16(7):e63902. https://www.cureus.com/articles/239902
Hermansson H, Kumar H, Collado MC, Salminen S, Isolauri E, Rautava S. Breast Milk Microbiota Is Shaped by Mode of Delivery and Intrapartum Antibiotic Exposure. Front Nutr. 2019 Feb 4;6:4. doi: 10.3389/fnut.2019.00004. PMID: 30778389; PMCID: PMC6369203. https://pmc.ncbi.nlm.nih.gov/articles/PMC6369203/
Mayo Clinic Health System. (2022). Managing plugged ducts and mastitis while breastfeeding. https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/managing-plugged-ducts-mastitis-when-breastfeeding
Huang, T., et al. (2022). Effect of breast milk with or without bacteria on infant gut microbiota. BMC Pregnancy and Childbirth, 22:595. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-022-04930-6
Boudry, G., et al. (2021).The Relationship Between Breast Milk Components and the Infant Gut Microbiota, 8:629740. https://www.frontiersin.org/articles/10.3389/fnut.2021.629740/full
Arroyo, R., et al. (2010). Treatment of infectious mastitis with Lactobacillus fermentum and Lactobacillus salivarius: A randomized trial. Clinical Infectious Diseases, 50(12), 1551–1558. https://doi.org/10.1086/652763
KellyMom. (2023). Lecithin treatment for recurrent plugged ducts. https://kellymom.com/nutrition/vitamins/lecithin/
Drugs and Lactation Database (LactMed). (2021). Lecithin. National Library of Medicine (US). https://www.ncbi.nlm.nih.gov/books/NBK501772/
Clemente JC, Manasson J, Scher JU. The role of the gut microbiome in systemic inflammatory disease. BMJ. 2018 Jan 8;360:j5145. doi: 10.1136/bmj.j5145. PMID: 29311119; PMCID: PMC6889978. https://pmc.ncbi.nlm.nih.gov/articles/PMC6889978/
Kho, Z. Y., & Lal, S. K. (2018). The human gut microbiome – a potential controller of wellness and disease. Frontiers in Microbiology, 9:1835. https://doi.org/10.3389/fmicb.2018.01835